A collective responsibility for a safer world
Infectious medical waste: the invisible diseases threatening healthcare workers
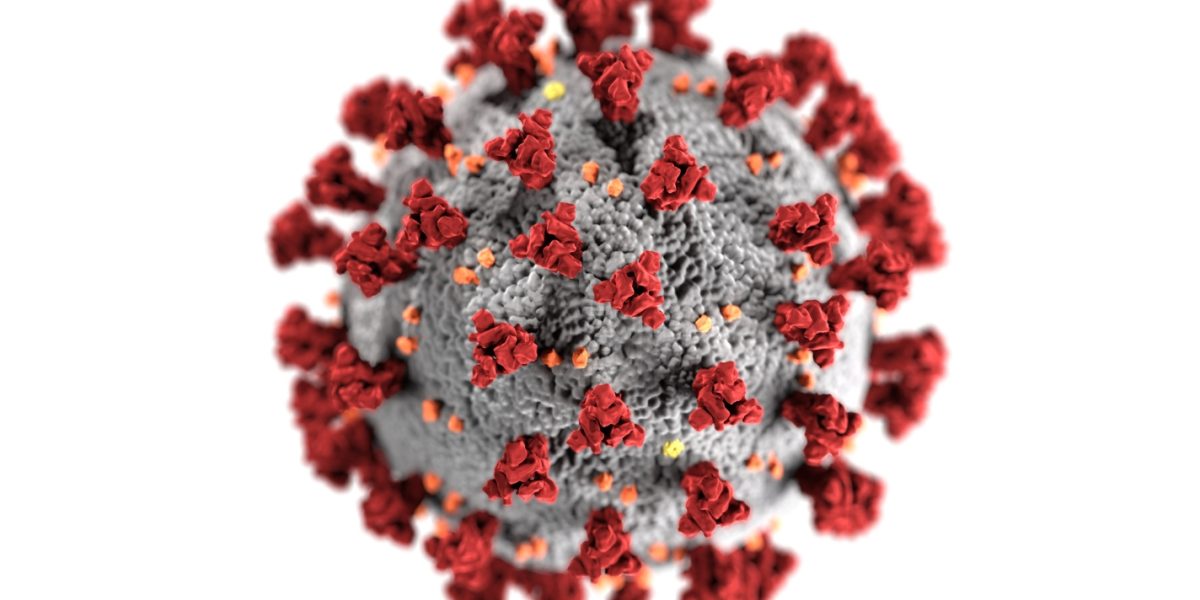
Every day, tonnes of infectious healthcare waste are generated in hospitals, clinics, laboratories, care homes, and even private homes. Behind a seemingly harmless used needle or soiled dressing may lurk invisible yet formidable pathogens. Hepatitis, HIV, antibiotic-resistant staphylococci… the dangers are real and often underestimated. In a global context of heightened health vigilance, understanding and controlling these risks has become a public health priority.
Waste unlike any other
Not all waste resulting from healthcare activities is created equal. Infectious Healthcare Waste (IHW) – in French, Déchets d’Activités de Soins à Risques Infectieux (DASRI) – includes materials that may contain microorganisms capable of causing infections in humans or animals. This waste is produced in various environments: hospitals, GP surgeries, vaccination centres, diagnostic laboratories, and also during home care procedures.
It includes used needles, syringes, catheters, dressings, gloves, swabs, contaminated test tubes, and even anatomical parts. Its handling requires utmost care, as improper disposal or contact can expose individuals to potentially incurable infections.
Transmission methods: infection at your fingertips
The key danger of IHW lies in its capacity to transmit infectious agents. Unlike household rubbish, this material can remain hazardous for hours or even days, depending on the conditions.
Contamination may occur in several ways:
- Through needlestick injuries or cuts from contaminated sharp objects.
- Through contact with broken skin or mucous membranes, particularly when handling waste without protection.
- Via projection or splatter of biological fluids during transport or sorting.
- By inhalation of contaminated aerosols during certain treatments or when opening non-compliant waste bags.
Each unprotected action can therefore turn into the starting point of a preventable infection.
Silent but serious diseases transmitted through hospital waste
A number of infections can be contracted via IHW. Some are well-known to the general public, while others are less so. Below is a summary of the main infectious risks identified in healthcare field:
| Pathogen | Associated disease | Mode of transmission |
|---|---|---|
| Hepatitis B virus (HBV) | Hepatitis B | Blood, needlesticks, skin contact |
| Hepatitis C virus (HCV) | Hepatitis C | Blood, needlesticks |
| Human Immunodeficiency Virus (HIV) | AIDS | Blood, bodily fluids, needlesticks |
| Methicillin-resistant Staphylococcus aureus (MRSA) | Nosocomial infections, sepsis | Skin contact, aerosol |
| Mycobacterium tuberculosis | Tuberculosis | Aerosol, indirect contact |
| Clostridium difficile | Infectious colitis | Faecal contact via contaminated objects |
| Candida albicans | Fungal infections, opportunistic infections | Contact, immunosuppression |
The most exposed professions, those most in contact with medical waste
Contrary to popular belief, doctors are not the only ones at risk. Many incidents involving IHW affect professionals who often work behind the scenes:
- Nurses and care assistants, who handle waste directly at its source.
- Cleaning and waste collection staff, often less trained yet in daily contact with IHW.
- Waste treatment technicians, responsible for sterilisation, transport, or shredding.
- Patients and home caregivers, particularly when self-care procedures are poorly supervised.
According to the World Health Organization, more than 2 million sharp-related injuries are reported each year among healthcare professionals worldwide, resulting in approximately 66,000 hepatitis B infections, 16,000 hepatitis C cases, and 1,000 HIV infections.
Prevention, training, innovation: pillars of responsible management
To mitigate these risks, several key measures exist and must be deployed at all levels of the care and waste management chain.
- Use standardised, secure containers
IHW must be disposed of immediately after use into rigid, leak-proof, sealed and certified containers to prevent spills or accidental injury. - Educate and raise staff awareness
Regular, role-specific training is essential to reinforce good practices, safety protocols, and the importance of correct sorting. - Adopt eco-friendly treatment technologies
Incineration, long used as a disposal method, is now criticised for its pollutant emissions. Innovative alternatives exist: machines developed by companies like Ecosteryl use a combination of microwaves and dry shredding to effectively neutralise pathogens — without combustion, water, or toxic emissions.
These solutions not only significantly reduce the medical sector’s carbon footprint but also ensure biosafety by sterilising infectious waste thoroughly.
A shared responsibility for global health
The management of infectious medical waste is a silent but vital challenge. It calls upon the responsibility of healthcare institutions, public authorities, manufacturers, and each healthcare worker. By reducing transmission risks, adopting sustainable technologies, and fostering a culture of prevention, we can ensure that medical waste does not become a vector of contamination.
At a time when health systems are under strain from pandemics, economic crises, and environmental pressures, rethinking how we handle IHW is more than just a necessity — it’s a commitment to global health.
Sources :
- World Health Organization (WHO) – Healthcare Waste Management
- INRS France – Risks Related to Healthcare Waste
- Institut Pasteur – Hepatitis B and C Transmission
- French Ministry of Health – IHW Management Guide




